I started the previous blog by referencing Richard Rumelt's great book Good Strategy, Bad Strategy which says this:
“Unfortunately, good strategy is the exception, not the rule. And the problem is growing. More and more organizational leaders say they have a strategy, but they do not. Instead, they espouse what I call bad strategy. Bad strategy tends to skip over pesky details such as problems. It ignores the power of choice and focus, trying instead to accommodate a multitude of conflicting demands and interests. Like a quarterback whose only advice to teammates is “Let’s win,” bad strategy covers up its failure to guide by embracing the language of broad goals, ambition, vision, and values. Each of these elements is, of course, an important part of human life. But, by themselves, they are not substitutes for the hard work of strategy.”
And defines the core of good strategy thusly:
“The kernel of a strategy contains three elements: 1. A diagnosis that defines or explains the nature of the challenge. A good diagnosis simplifies the often overwhelming complexity of reality by identifying certain aspects of the situation as critical. 2. A guiding policy for dealing with the challenge. This is an overall approach chosen to cope with or overcome the obstacles identified in the diagnosis. 3. A set of coherent actions that are designed to carry out the guiding policy. These are steps that are coordinated with one another to work together in accomplishing the guiding policy.”
How can we compare NHS strategy to these criteria?
Not well is a good summary. Epic fail might be more accurate. Malcolm Tucker would, more colorfully, go straight to clusterfuck or omnishambles. Both the NHS plan and recent documents like the 2022/23 NHS mandate are guilty of "Let's win" as a statement of strategy. His sentence "...bad strategy covers up its failure to guide by embracing the language of broad goals, ambition, vision, and values." could be a review of either document.
On his more detailed definition of what good strategy looks like, NHS guidance fails on all three criteria. The NHS has studiously avoided diagnosing "what the problem is" for the system as a whole and has, for much of the last decade at least, explicitly promulgated strategy that is contradicted by strong evidence that already exists (concrete examples later).
The tenor of specific mandates has avoided stating any clear policy for meeting whatever challenges there are (which is much easier when you don't have a diagnosis). In fact a good description of the latest mandate is that "everything is a priority". But, to paraphrase Syndrome in the greatest Pixar movie, the Incredibles, "If everything is a priority, nothing is".
And as for aligning actions to the goals of strategy or the stated intentions of the strategy, the NHS has won the World Incoherence championship at least 12 years in a row (more specific examples later).
But let's go through Rumelt's three parts of good strategy and assess the NHS against them.
What is the biggest barrier to improvement? What is the diagnosis?
The NHS has big problems. Some of the symptoms of those problems are very visible:
Long and worsening waits for elective treatment
Apocalyptic waits for emergency treatment
Overloaded GPs with a workforce rapidly losing faith in the system
Repeated cover-ups of scandals about care quality in hospitals
Insiders and experts might add others to this list, but these are the big symptoms that are most obvious.
But many of these have been obvious for most of the last decade.
Some, like GP overload, have even been the subject of significant plans. We've been trying to increase GP numbers since Jeremy Hunt was SoS but Extra trainees don't appear to be arriving fast enough to compensate for the losses in experienced GPs.
We have also had plans to tackle A&E waits. But the one common feature of all of them is they ignore known diagnoses of the causes of waits. Keith Willet spent a lot of the decade promoting "channel shift" (which in practice meant a lot of efforts to divert patients away from major A&Es) despite repeated analysis suggesting that the divertible "minor" patients were not the cause of the problem (see this analysis from Monitor) and, even if we could make diversion work (we apparently can't) this would not influence the apocalyptic current performance.. And, worse, NHSE have proposed changing the published metrics for A&E departments in ways that obscure their performance rather than help fix it (see my analysis of the proposals).
And these are just the tip of the iceberg. The NHS has had an ambition for decades to shift care away from hospitals into the community. If anything, hospitals now have a stronger hold on the budget than they used to (see some of the analysis on this in the FT article here). The idea of putting more effort into prevention has been stated for years. Yet the budget has repeatedly been an easy target for cuts.
As the NHS has struggled to recover from covid, there have been repeated initiatives trying to treat the symptoms. Reduce ambulance handover delays! Reduce long waits in A&E! Reverse the climbing elective waiting list! What characterizes these more than anything else is the complete lack of any overarching diagnosis explaining what the problem is. Strategy is literally the same as a football manager whose strategy and tactical advice consists entirely of "win the next match".
What these fragmented attempts to treat symptoms have in common is the lack of any clear diagnosis of the underlying problem causing the symptoms or preventing improvement from happening. If a patient presents to a doctor with "headaches" they could just have a headache or a hangover. But, sometimes, they have meningitis, a brain tumor or a concussion. Treating the symptom works for some of those but not others depending on the actual diagnosis. If the doctor treats the symptom without trying to get a better diagnosis, many patients will be fine but some will suffer harm. The NHS seems to perpetually focus on trying to treat the symptoms and completely ignorant of the risks of an incorrect diagnosis.
But this leap to treating the symptom without getting a better diagnosis is exactly how NHS plans have tried to deal with the big symptoms for more than a decade.
What is the guiding policy?
In the absence of a convincing diagnosis of where the big problems are, policy is–obviously–somewhat untethered to reality. This is a problem. A big problem.
It would be unfair of me to say that the early 2019 NHS Long Term Plan has no analysis or no ambitious goals. But it is stymied by a lack of focus, many critical omissions and a naive belief that structural and financial changes can achieve actual improvement. And many of the ambitious actions proposed there have not resulted in actual changes in the real NHS.
The plan, for example, promised 5,000 more GPs. We don't even have more GPs. It has a section on improving leadership and recognises a shortage in the pipeline of potential leaders. But says nothing about management or the chronic lack of management capacity, despite this being a major cause of the deficit in the leadership pipeline. And it promises more cuts in the name of "efficiency" that are likely to reduce the number of managers.
Unusually, it recognises a long term failure to invest in capital as a problem. But promises changes that didn't materialize in the spending reviews or budgets between 2017 and 2021. And, though there was a big commitment in 2022 to invest more in capital, a lot of that is earmarked for "new" hospitals or community diagnostics (a good idea, BTW), the core budget for improvements in existing units is little changed and there is nothing in the proposed changes to the capital regimen to prevent the repeated capital underspends or transfers to revenue that have shrunk the capital budget for most of the last decade. Two developments since the start of the 2022/23 financial year suggest backsliding on capital commitments. New rules to constrain FTs are being proposed so the center can avoid an arbitrary treasury rule about total spend (a rule which is a major reason for previous problems in investing enough capital). And the center is already trying to claw back some of the budgets promised just a few months ago.
So, overall, the strategy lacks good diagnosis and any focus on a handful of big problems.
What is the plan?
The 2022/23 mandate is probably even worse. Here are the focus areas from the appendix:
More Nurses
More GP appointments
40 new hospitals
Improved post pandemic performance in A&E and elective waits
Supporting leveling up and health inequalities
Better access to community and primary care
Mental health improvement
More technology
Better outcomes in 6 areas prioritized in long term plan
Better outcomes for long term conditions
Better maternity outcomes
Better support for workforce
Financial balance
All shall have prizes! What I struggle to see is what has been left out. Everything seems to be a priority. Focus is like something the authors needed to look up in a dictionary but couldn't find because they lost their reading glasses.
What is most disturbing is the absence of any idea that the NHS is a system where the parts interact. This has multiple implications. For example, there is no fixing ambulance performance or A&E performance without tackling exit block from hospital beds. That might suggest a focus on that before demanding improvement in A&E and ambulances. There is no sign of that focus. Also, to actually achieve improvements, the interactions between different components of the NHS need to be considered. For example, improved performance might require more capital spending and more support staff to increase front line productivity. Getting that mix right implies a different analysis of the problem (which is completely absent) and a different mix of spend in the budget. There is no sign of that either. If anything, the stated goals assume we can have more of everything without having to reallocate any money: so, more nurses, more hospitals, more technology, more GP appointments…
Hence my complaint that the apparent logic of the priority list is not achieving anything but pleasing every possible group by telling them that they are a priority (I said this on Twitter and got some pushback claiming the plans are developed by people with good, not cynical motivations). But words are cheap, action is expensive and a homeopathic level of focus is not any more effective in strategy than it is in medicine. Everything Everywhere All At Once is the best movie of the millennium so far, but it is not an effective plan that will focus NHS effort on solving the big problems.
So we seem to have an NHS strategy that misses all three of Rumelt's essential elements of a good strategy.
It might be even worse than that. Let's look at some possible analyses of specific known issues and how the NHS has handled them.
The perpetual mismatch between known problems and the actions required to tackle them
The absence of a clear diagnosis of the biggest problems and the homeopathic level of focus in plans have consequences. One of the most serious is a repeated failure to match action to the goals. Here are some specific examples.
The NHS has long recognised the goal of doing more in the community and more prevention rather than treatment. But neither have seen much action. This analysis from the Kings Fund at the start of 2018 suggests the goal has failed to move the needle on action:
"Our recent work on general practice and district nursing has shown that the policy narrative about the need to transfer care from hospital to community health services is not being accompanied by a similar transfer of resource."
And the Health Foundation, reviewing the prospect for the new Office of Health Improvement and Disparities (the successor to Public Health England) reported:
"The public health grant has been cut by 24% on a real-terms per capita basis since 2015/16."
And the Kings Fund analysis of the 2021 spending review argues:
"the [public health] grant will be maintained in real terms over the next three years – a decision described as ‘unfathomable’ by public health leaders, who have played a crucial role in the response to and recovery from the Covid-19 pandemic. On a like-for-like basis the public health grant has already been cut by 24 per cent in real terms per person since 2015/16. And it is hard to see how public health services (and the people who deliver and use them) will not come under more intense pressure over the next three years."
So the NHS thinks–as it has for decades–that improving public health is a priority. Except when it comes to allocating money, when it is Cinderella, stuck in the basement with a dirty second hand dress.
What about emergency care? That has become a very visible sign of NHS failure with perhaps 8% of attenders at A&E waiting 12hr for discharge or admission. This alongside very long ambulance waits. This is a priority, isn't it?
Here we have a different kind of problem. It isn't the allocation of money or at least not the total amount spent. It is a persistent set of policies that fail to identify the root cause of long waits in A&E (which are, in turn, the root cause of ambulance waits).
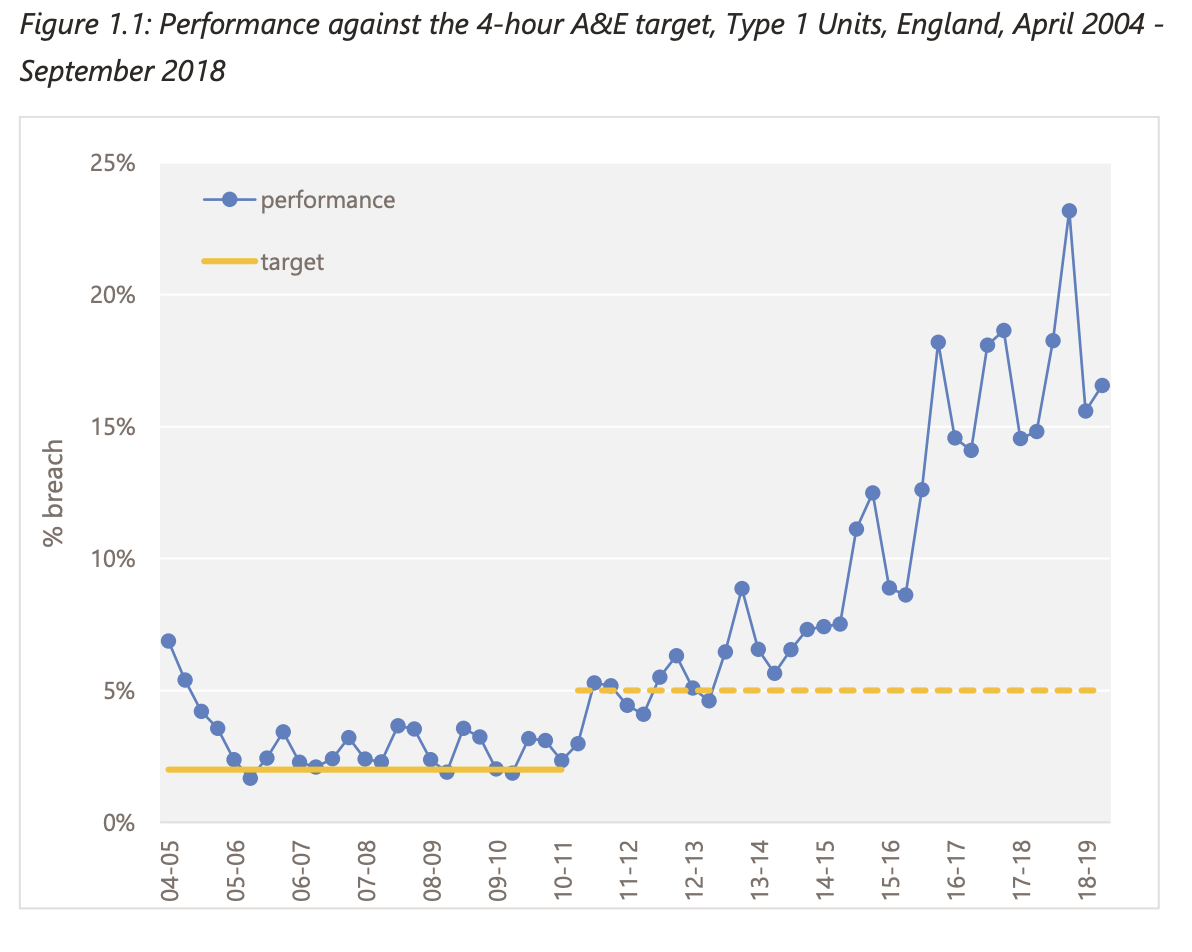
And it isn't a new or primarily covid-related issue: things have been declining since Lansley's unwise decisions to threaten to abolish the target and then to relax it:
Note the immediate decline in performance coinciding with Lansley relaxation (presumably to make it easier to meet, spoiler, it didn't) in this Strategy Unit chart. Things have kept declining ever since.
The causes of long waits are, at least in principle, well known. I was writing on the topic in 2013, writing about them in 2016 and again in 2017. Monitor did an excellent review of the evidence in 2015.
The Monitor report contains a handy picture of what their analysis showed at least for the parts of the decline that could be explained:

Note that things inside A&E department itself explain nothing. Nor do the numbers of discharged patients or total attendance. Pay attention to these observations, there will be a quiz at the end.
Monitor remarked:
"Our view is that the available evidence for the half of the decline that can be explained is strong enough to underpin policy, and that the findings of the analysis point to particular policy interventions that are likely to help prevent the decline from occurring again."
Policy, however, has rolled on apparently oblivious to this analysis. Two major things have dominated it.
One is the idea that the problem can be tackled by "channel shift" (which means diverting patients to other services). According to Monitor's analysis (and many by me and other experts) this would make no difference at all.
The second is that we need to measure A&E performance in a different way. The 4hr target is so last decade, according to proposals first put forward in 2019. The logic behind these alternative metrics is shockingly dodgy. A better explanation for them is that they are designed to minimize the opportunity for bad news when performance is published every month. These proposals have still not been implemented (thank fuck) but they have been piloted in 14 trusts. I wonder why the results from the pilots have not been published?
So we have a major area of the NHS where performance has been declining for a decade to a level where instead of getting most patients through A&E in 4hr, England struggles to get 90% through in 12hr. And Those long waits are, most likely, killing patients as a recent analysis in the Emergency Medicine Journal suggests.
But, while policy and NHSE plans are keen to say this is a priority, the policy ignores credible diagnoses and directs attention to other actions. One of which can't work if the diagnosis is correct, the other of which can only hide the problem, not fix it.
Without diagnosis, focus and coherent action there is no hope for improvement
All strategy is futile if it isn't based on a good diagnosis of the barriers to achieving the goals. And, even if there is a diagnosis, a lack of focus on the top problems will dilute the efforts to nothing can be achieved anywhere. On top of that, if you don't match the plan with action, your goals will remain beyond the horizon if not beyond the heat death of the universe.
Since NHSE strategy and policy seems to have striven to make all three of those errors at the same time, I'm not full of hope.
We have clear examples where the diagnosis is wrong (A&E policy). The prioritization seems to be based on the idea that, if one priority is good, two would be better and 13 would be amazing (the 2022/23 mandate).The mandate priorities have single handedly reintroduced the idea that homeopathic dilution is effective into the NHS. And, even when there is a priority, clearly stated, the plan takes money away instead of adequately funding the priority area (capital spend and public health spend).
NHS Strategy is–to paraphrase Douglas Adams–a shit show, a clusterfuck of incoherent ideas, the entire set of pejorative descriptions from every major thesaurus in the galaxy.
So what?
Many documents and statements about strategy by NHSE seem to be based on the principle that if they declare that every major area of NHS activity is a priority, this will make everyone happy and motivated to achieve improvement in their domain. Or, if we tell everyone that they are doing a good job (with claims like "we have treated a record number of patients, well done") this will motivate them to improve performance. The trouble with this attitude is that, when the problems are large and manifest to all the staff, telling them things are OK and could get better just demotivates everyone by strongly signaling that the leadership either hasn't reached their clue quota on knowing what the problems are or hasn't any intention of doing anything significant about those problems. When you are in a shit storm, prescribing more anti-constipation meds is rarely the right approach. When the car has four flat tyres, praising the driver for how far they have managed to travel already is an unwise approach.
We may be very close to the point where more boosterism from NHSE will precipitate a complete collapse of the NHS. Everyone knows they are sinking into a sewage filled quagmire. In those circumstances, boosterist statements signal the opposite of their apparent intent. Not "things will soon get better" but, rather, "we are so clueless about the problem that all hope is lost". The exodus of staff from GP land, for example, is already apparent. And may rapidly get worse. What they–and many other staff groups need–is not more boosterism but a clear headed, well argued statement that the center understands what the problem is and will focus on fixing it. They don't need fake promises that miracle cures will fix everything next year: they need hope that the underlying causes of the problems are now recognised and that (perhaps after several years of effort) things will be better. There is no prospect of hope when boosterism squeezes out all realistic analysis of just how bad things are and how hard they will be to fix.
Far better to do the analysis of what the root causes of the apocalyptic state of the system actually are. Then openly admit them alongside a clear commitment to focus the NHS on tackling the big ones instead of pretending to tackle them all. Focus and honesty might create enough hope that things can be fixed that the impending apocalypse might be avoided. More "strategy" based on boosterism and with all the focus of a clumsy child's first photograph might turn the current apocalypse into armageddon in the near future.